US-Greater trochanter injection vs standard ED care: a thought experiment
/Can we improve care of acute exacerbations of chronic pain, reduce system cost, and limit opioid prescriptions all while increasing patient satisfaction. Bonus! with appropriate CPT /RVU coding we can actually get paid to do the right thing for our patients ( some of them anyways!)
Example case from St Somewhere ED: A 40 something man with known lumbar disc disease presents to the ED in severe pain; near agony. He is polite, but seems focused on pain medicines. He is here with his mom who comes into the hallway to ask if we are going to give him "something for pain."
After a thorough exam confirms sciatica without red flags the initial provider orders morphine IV. Perfectly reasonable--he is on ibuprofen, gabapentin, and Norco at home, now he is worse--escalating the analgesia seems like the right thing to do.
But is going to intravenous opioids the only way to escalate analgesia in the ED? No!
I ask for a few minutes to talk with patient in more detail and come up with an alternate plan. In the meantime we order ibuprofen, acetaminophen, and a 900mg does of Gabapentin orally.
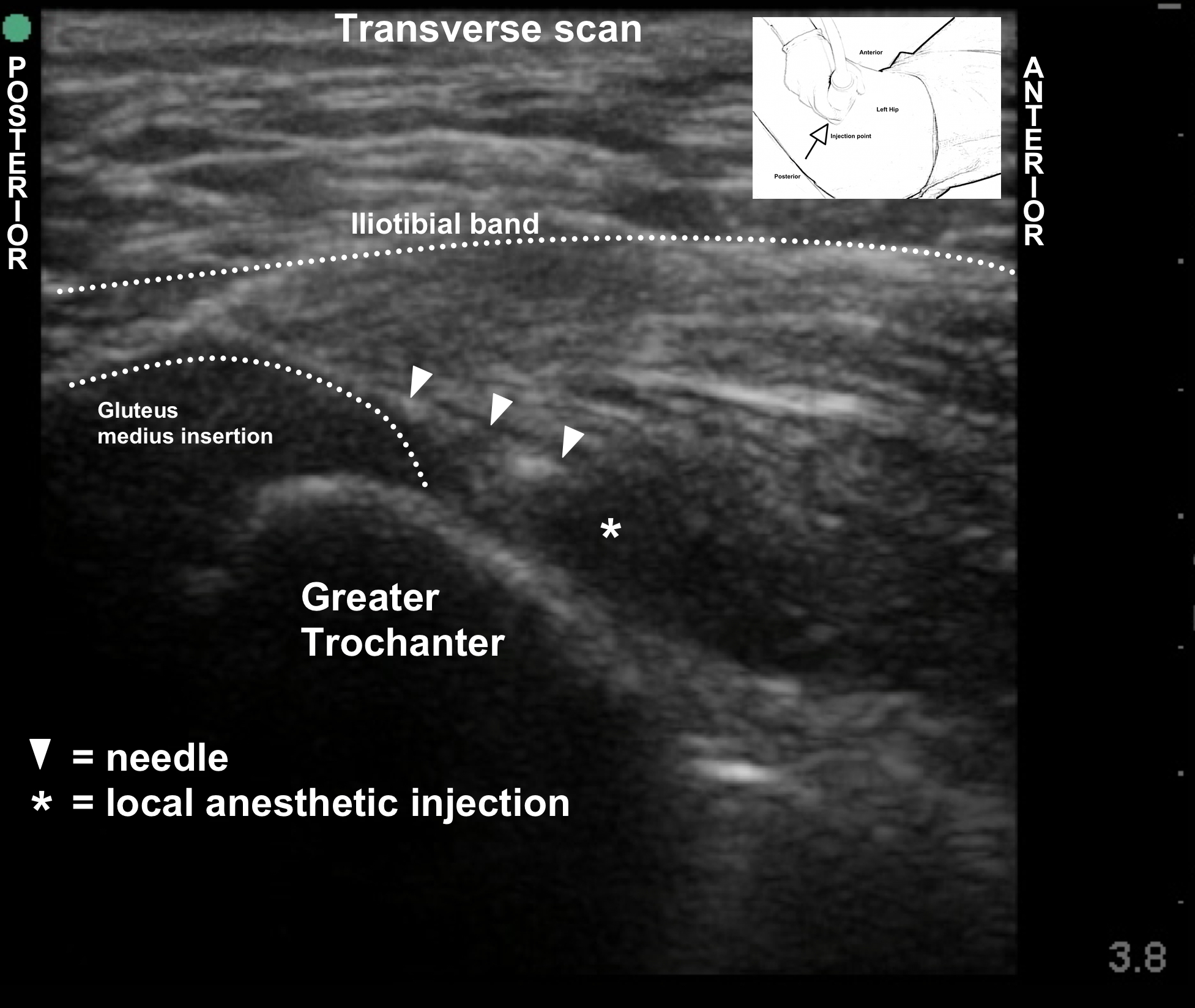
I talk with him, and it becomes clear the chronic back pain has lead to irritation of the greater trochanter of his hip--so called greater trochanter syndrome. We identified the greater trochanter on ultrasound and quickly performed an ultrasound-guided injection of local anesthetic and corticosteroid.
His pain was relieved completely and he spontaneously offered "I went to ANOTHER HOSPITAL and all they did was give me morphine that made me feel sick and didn't do anything....I learned so much about my pain here and this injection was a miracle."
He was discharged without any opioids, happy, on the path to active engagement of his pain, and hopefully, getting better. With the patient feeling the glow of zero pain without a narcotic haze, he is able to actually hear education around active engagement of pain, daily exercise, stretching and weening off the Norco all together.
This was SO much more effective and LESS expensive than the alternate scenario:
47yoM with known disc disease presents to the ED in severe pain; near agony. As emergency physician I quickly determine there are no red flags and no urgent issue besides pain. The more time unstructured time I spend with the patient, the less time I have to see other patients. There is nothing to do besides offer tylenol or ibuprofen ( which he already takes and says doesn't work) or give him a quick shot of opioid so he feels comfortable enough to leave.
AND best case scenario follow up
Refer him to pain specialist to be seen in 2wks-6mos to never, to be diagnosed with greater trochanter syndrome and given an injection. ( And a lot more, but you get the point--why wait?)