Treatment of Intractable, fulminant, cyclic, out-of control...nausea vomiting and abdominal pain (...you are an ED doc, you know what I mean)
/No opioids, no benzos, no admission = victory

But as the regulatory eagles ?buzzards circle ever closer on our practice, what is the dart? Is it analgesia?, anxiolysis? If it is procedural sedation then what is the procedure?
An informal pole of some the bright lights in emergency medicine suggests the safest and most appropriate way to practice is:
Continue considering the 5mg IM versed ( or other benzo as a light sedation ) No need to break out the packet or fire up the EMR sedation module for this...whew!
BUT...when upping the ante with the dart of ketamine at the 4-5mg/kg IM, (often after who know how much preceding medication), bite the bullet and consider this a bona fide "procedural sedation."
1. You can skip all the pre-sedation evaluation due to urgent patient need.
( Sir, I see you are trying to eat through the straps on your arm, but could you tell me when last ate?)
2.The procedure is "immobilization for safety."
3. Monitor and document as you would any other sedation, ideally with ETCO2 & and pulse ox. Pay special attention to prevention of mechanical obstruction. (The idea is with ketamine you will keep breathing but may not have the muscle tone to independently straighten out the neck to keep the airway patent.)


"It should be noted that according to the league table opioids may be less effective for acute pain than medicines with other different mechanisms of action"
The royal college of Anesthetists; Faculty of Pain Medicine 2016



Dex is a very powerful anti-inflammatory and analgesic medicine. In the ED, we see it work for back pain and pharyngitis everyday. It is also a great option for dental pain working by the same mechanisms. Plenty of literature on wisdom tooth extractions to support this approach. We have no data from the ED at this point, but it is hard to develop an argument that the pain and swelling of acute dental pain in the ED should NOT respond in a similar fashion as the perioperative dental studies. The studies below are a good place to start a lit review.
Reminder how-to on inferior alveolar block
One more procedure we can offer our patients. Learn more here.
bakers aspiration panel from andrew herring on Vimeo.
The pecs II block is based on the concept that the intercostal nerves can be blocked as they travel through the intra-muscular planes of the upper thorax. This let's you avoid intercostal or paravertebral blocks. It is very similar to the TAP block concept.
Developed by breast surgeons, it works for the upper chest and axilla, importantly it gets the intercostobrachial nerve.
Here is Podcast I recently did with the Ultrasound Podcast Team
* Intralipid - don't know what this is? Don't have it ? Don't know where it is? Don't do the block! You have some homework to do first!
ASRA guideline
1. The short procedure you plan on doing yourself: perfect for shoulder reductions
-3% Chloroprocaine
~Why? non-toxic with a 40 sec half-life in the blood, rapid on ( 15 min ) and gone in about 60-90minutes
2. The more complex procedure that may be delayed or where you must depend on a consultant who may show up late: the abscess with cellulitis getting admitted
- 1.5% Mepivacaine
- Why? Proven track record with for 2-3 hours dense anesthesia and 8 hours analgesia. Similar toxicity to lidocaine--potentially serious, but lower risk than ropiv or bupiv.
- Alternative = 2% lidocaine ( 1% also works, though more inconsistent )
3. Long bone fracture analgesia: the hip fracture
- 0.5% Ropivicaine or 0.25% Bupivicaine
- Why? long acting, powerful local anesthetics that should be used with caution due to potential for cardiovascular toxicity.
In the low acuity section of any emergency department in the country there are many patients presenting with chronic pain, most commonly back pain, knee pain, hip pain. Many patients where unwittingly steered away from actively engaging their pain with exercise, rehabilitation, and self-motivation towards a passive approach that promotes a sense of helplessness and reliance on medications. Opioids play right into this dynamic and in some patients promote passivity, increasing disability and overall worsening in function.
Interestingly, smoking is a powerful risk factor for developing chronic pain. The mechanisms are complex and discussed in detail in the article by Shi et al below, but the association is clear. In my practice I found putting a clear boundary on the amount face-to-face time I spent discussing opioid scripts with my patients opened up time to spend discussing issues I know are truly of benefit to them like smoking cessation and exercise.
JAMA recently published an article by Elbert et al. ( also below) on a the success of varenicline in helping patients quit smoking. Given the evidence and increasing options available to us, smoking cessation should be considered a core component of any initiative to improve emergency department treatment of pain and promote rational use of opioids in chronic pain.
Emergency medicine is medicine of the unforeseen. Ultrasound-guided regional anesthesia gives the emergency provider an expanded set of capabilities to manage trauma beyond sedation. Integrating UGRA into emergency care is complex and requires establishing a close relationship with participating trauma, orthopedic, and anesthesia consultants. However, once established the possible benefits to initiating a multimodal plan integrating regional anesthesia as close to the time and place of injury is clearly of benefit to trauma patients in the emergency department
Can we improve care of acute exacerbations of chronic pain, reduce system cost, and limit opioid prescriptions all while increasing patient satisfaction. Bonus! with appropriate CPT /RVU coding we can actually get paid to do the right thing for our patients ( some of them anyways!)
Example case from St Somewhere ED: A 40 something man with known lumbar disc disease presents to the ED in severe pain; near agony. He is polite, but seems focused on pain medicines. He is here with his mom who comes into the hallway to ask if we are going to give him "something for pain."
After a thorough exam confirms sciatica without red flags the initial provider orders morphine IV. Perfectly reasonable--he is on ibuprofen, gabapentin, and Norco at home, now he is worse--escalating the analgesia seems like the right thing to do.
But is going to intravenous opioids the only way to escalate analgesia in the ED? No!
I ask for a few minutes to talk with patient in more detail and come up with an alternate plan. In the meantime we order ibuprofen, acetaminophen, and a 900mg does of Gabapentin orally.
I talk with him, and it becomes clear the chronic back pain has lead to irritation of the greater trochanter of his hip--so called greater trochanter syndrome. We identified the greater trochanter on ultrasound and quickly performed an ultrasound-guided injection of local anesthetic and corticosteroid.
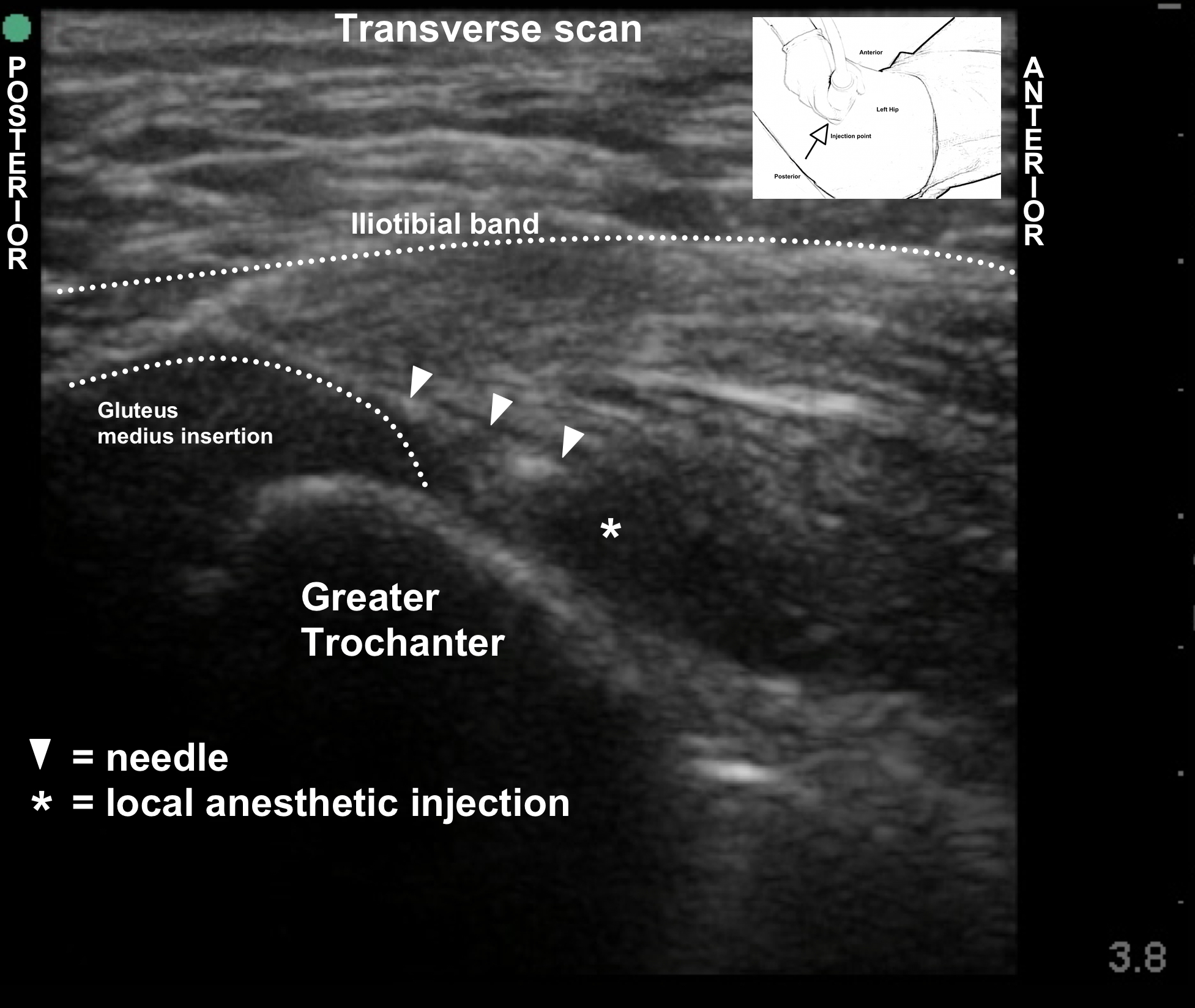
His pain was relieved completely and he spontaneously offered "I went to ANOTHER HOSPITAL and all they did was give me morphine that made me feel sick and didn't do anything....I learned so much about my pain here and this injection was a miracle."
He was discharged without any opioids, happy, on the path to active engagement of his pain, and hopefully, getting better. With the patient feeling the glow of zero pain without a narcotic haze, he is able to actually hear education around active engagement of pain, daily exercise, stretching and weening off the Norco all together.
This was SO much more effective and LESS expensive than the alternate scenario:
47yoM with known disc disease presents to the ED in severe pain; near agony. As emergency physician I quickly determine there are no red flags and no urgent issue besides pain. The more time unstructured time I spend with the patient, the less time I have to see other patients. There is nothing to do besides offer tylenol or ibuprofen ( which he already takes and says doesn't work) or give him a quick shot of opioid so he feels comfortable enough to leave.
AND best case scenario follow up
Refer him to pain specialist to be seen in 2wks-6mos to never, to be diagnosed with greater trochanter syndrome and given an injection. ( And a lot more, but you get the point--why wait?)
Small study suggests 8 IV dexamethasone along with 30ml 0.5% Bupivacaine prolongs interscalene analgesia from a mean of 13 hours to 25 hours for patients undergoing ambulatory upper extremity surgeries. Why this works no one really knows. More data is needed but certainly at this point looks promising that dex will significantly prolong blocks. Should this become standard for hip fracture patients presenting to the ED?



Selecting the right local anesthetic is a bit of art form. There are many different cocktails is use, each with their own ardent supporters. The science is hard to interpret given the many factors that go into creating a successful block. Putting it all together this is my ideal line up for local anesthetics in emergency practice:
3% 2-Chloroprocaine for ultra-short blocks in the 60-90 minute range. This is perfect for reductions or procedures where you would like a brief block. As an ester rapidly metabolized in the blood ( <60 second half-life), the risk of toxicity is very low. This low toxicity allows safe use of a high concentration ( 3%) that likely contributes to the very fast onset of the block. Example would be an intersalene block for shoulder reduction
Perfect for intermediate blocks when a several hour window of surgical level anesthesia is needed. Fast onset of 2-3 hours of dense surgical anesthesia. Consultants can be unexpectedly delayed, it is very very disappointing to have a block wear off just as the procedure is starting. Mepivacaine gives dense block and a nice window for this scenario. Mepivacaine has a strong following as a very consistent, low toxicity, amide local anesthetic. Mepivacaine does not have a strong vasodilatory affect and is typically used without epinephrine. Example would be an infraclavicular block for a distal radius fracture reduction and splinting.
Ropivacaine is structurally similar to bupivacaine with reduce cns and cardiovascular toxicity and some degree of preferential sensory blockade. It remains a powerful local anesthetic that should be used with caution, an understanding of the recognition and treatment of LAST with intralipid at hand. We use 40ml of 0.5% ropivacaine for hip fracture analgesia.
1% lidocaine is commonly stocked in the ED. At 1% this is probably the weakest local anesthetic you could use with acceptable clinical result. 1.5%- 2% is the more common dosage for lidocaine. Lidocaine has strong vasodilatory properties and is commonly used with epinephrine.
Bupiv is the strongest, most potentially toxic local anesthetic in use. Full LAST precautions are required. Blocks can be quite dense and of long duration > 10 hrs.
There is no consensus at this point, but animal study and in vitro evidence of neurotoxicity has sufficiently raised concerns that most are moving away from epi when possible.
To early to say. Has the potential to dramatically lengthen block duration. Unclear if dexamethasone needs to be injected perineurally or can be given IV with the block.
Further reading on the web about local anesthetics
26yoF struck by an auto as a pedestrian presented in with an obvious tib/fib fracture with her shoulder in this position:

The patient was confused, agitated with unbearable left shoulder pain. Any attempt to manipulate the shoulder was not tolerated. A preliminary FAST exam was concerning for possible intraperitoneal hemorrhage. The trauma team wanted to urgently pan CT scan the patient would not fit into the CT scanner gantry because of the arm position. A portable xray was obtained:

Diagnosis of luxatio erecta inferior shoulder dislocation with scapular fracture was confirmed.
After a thorough neurologic exam of the affected extremity found no deficits, pneumothorax was excluded on both CXR and POC US, the decision was made to place an interscalene brachial plexus block. Given the possibility of phrenic nerve paralysis and the generally undifferentiated condition, it was determined that a short acting blockade was preferable.

2-chloroprocaine is an ester with very low toxicity. This is reassuring in the high-pressure and potentially stressful acutely injured trauma patient scenario, where procedural errors are more common. Additionally, the onset of 3% chloroprocaine is very fast, potentially faster than any other option. The down-side is short duration of action, which is actually a benefit in cases like these where the physical reduction should dramatically reduce the pain, and a prolonged block could introduce concerns for evaluation of neurologic function or an inadavertent plexus associated, prolonged phrenic block could complicate management.

We prefer a stay-away approach where the needle tip is positioned underneath the middle scalene fascia and observed to spread into the interscalene groove, but we do not seek to position the needle tip between the nerve roots.
1) Sternocleidomastoid 2)anterior scalene muscle 3) middle scalene muscle 4) carotid artery 5) C5/C6/C7 roots 6) needle

10 minutes after an interscalene block was placed with 25mL chloroprocaine, the shoulder was easily reduced with minimal discomfort. To access the lateral neck, manual c-spine immobilization was used during the the block procedure. Post-reduction the patient was able to be comfortably positioned for pan CT scans which where negative for serious injury. During the hospital stay, the orthopedic injuries where repaired without complications.
Draining abscesses on the forearm can be a drag, injecting lidocaine into beefy red hot infected tissue hurts, gets messy, and it is easy to get suboptimal anesthesia even after all that stabbing.
Check out full tutorial video HERE

Posterior medial forearm abscess not improving with soaks and warm compresses; patient requesting to have it "opened up."
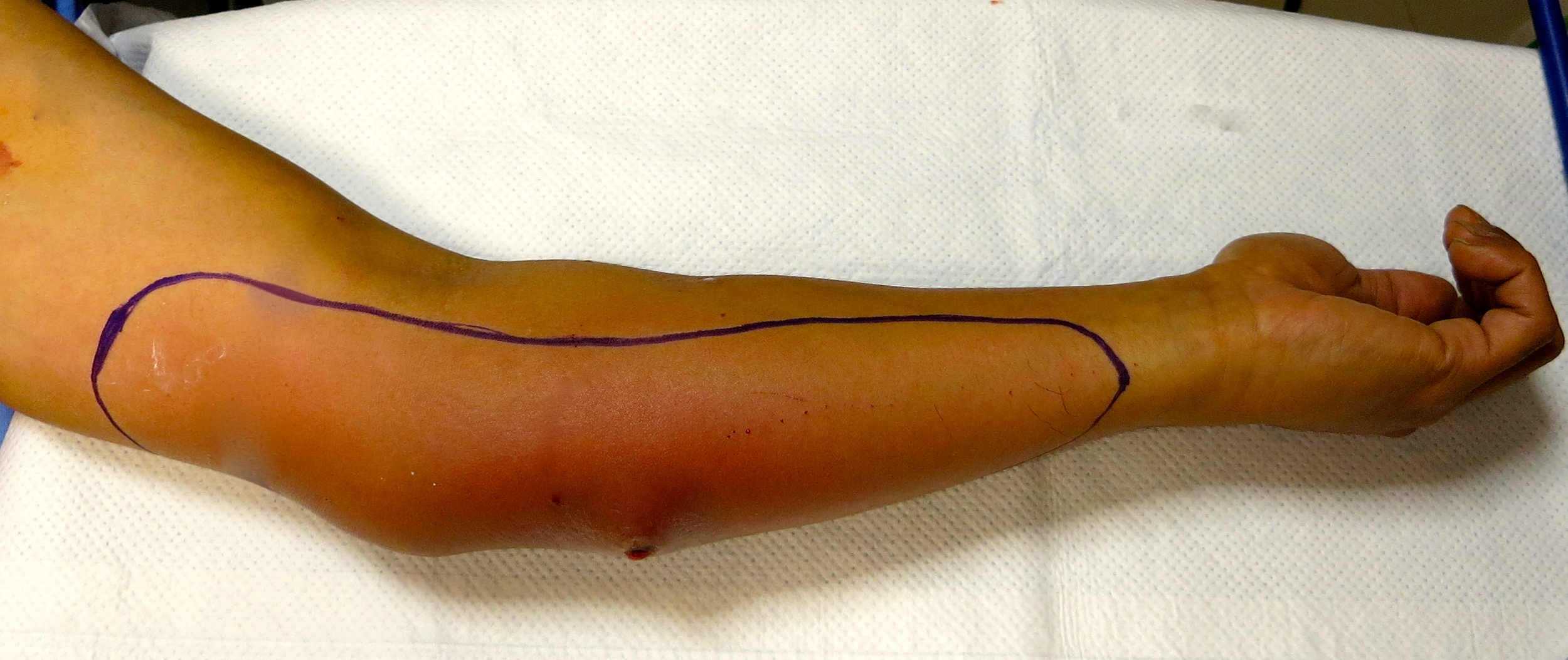
Area of anesthesia after an ultrasound-guided medial antebrachial cutaneous block was placed.

Download quick reference image HERE. The MACN arrises from the C8 and T1 nerve roots and travels within the medial cord. At the axilla it is quite superficial and runs down the medial aspect of the arm as a supeficial nerve in close proximity to the basilic vein. Its branches cover the medial aspect of the arm and forearm. When blocked at the mid-humeral level, the area of anesthesia shown is achieved. An in-plane approach with the arm outstretched is convenient. The nerve itself can be very superficial, its honeycomb appearance allows it to be distinguished from the surrounding connective tissue.

Painless incision and drainage.
Combine with a musculocutaneous block and you have the entire volar surface of the forearm covered. Remember if an injury is deep, involving the muscle, deep tendons etc...a brachial plexus block is required.
Ultrasound-guidance has recently been developed for the fascia iliaca block making it likely more of a reliable "3 in 1" block ( lateral femoral cutaneous, femoral, and obturator nerves) and the best option for acute hip fracture pain management in the ED.
For a detailed review of the anatomy check out this study HERE
Additional discussion HERE and HERE and HERE
Check out the TRAINING VIDEO HERE* and quick reference HERE.
Indication = Hip fracture
Risks = local anesthetic toxicity, hematoma in anticoagulated patients, intrperitoneal penetration has been reported, compartment syndrome possible but unlikely, use standard precautions to avoid infection, wrong side blocks, and nerve injury.

Procedure
1. Scan as you would for a femoral block and identify the femoral nerve and iliacus muscle just lateral to the femoral artery, be sure you are proximal to the bifurcation of the femoral artery.
2. Follow the contour of the iliacus muscle laterally and superiorly and rotate the probe to face the marker towards the umbilicus. To obtain the view and probe orientation seen in the figure below.
3. After placing a skin wheal with lidocaine. Use an in-plane approach aiming towards the umbilicus. If traversing the sartorius muscle, you may feel a "pop" as the needle encounters the fascia overlying the sartorius, then a second "pop" as it encounters the fascia iliaca. These pops are more likely to be felt with a blunt tip needle such as touhy.
4. The space underneath the fascia iliaca should open very readily with local anesthetic injection. As the space opens, the needle can be advanced with idea to direct the local in a proximal/cephalad direction.
5. This is a plane block; use large volume of dilute local anesthetic such as 0.25% bupivacaine or 0.5% ropivacaine. Use standard precautions to be prepared to recognize and treat LAST.
6. Mark the patient, document, and communicate with all providers participating in the patients care.
Check out the TRAINING VIDEO HERE and quick reference HERE.
As always practice safe regional anesthesia.
Regional Block Procedural Checklist
1) Patient is identified, 2 criteria. Appropriate identifying data entered in ultrasound machine.
2) Allergies and anticoagulation status are reviewed.
3) Consent for block and any associated procedure is confirmed.
4) Appropriate neurologic and vascular exam completed and documented.
5) Block plan is confirmed*, site is marked.
6) Necessary equipment is present, drugs are labeled.
7) Resuscitation equipment is immediately available: airway devices, suction, vasoactive drugs, lipid emulsion.**
8) Appropriate monitors are applied; intravenous access, sedation, and supplemental oxygen are provided, if indicated.
9) Aseptic technique is used: hand cleansing is performed, and sterile gloves are used.
10) “Time out” is performed before needle insertion.
Needling Technique
In-plane with real-time visualization of needle tip. Do not advance or inject if tip not clearly visualized.
Incremental injection after aspiration of 3-5mL at a time with confirmation of local spread on ultrasound. Total injection is 40mL 0.25% Bupivacaine.
Although the fascia iliaca block is a plane block, you should know how to monitor pressure using a compressed air technique.
Care hand-off
This will be a long acting block, it should be well documented and communicated to all teams participating in care. The leg should be splinted and protected.
*erratum - in the training video, I mistakenly referred to 2-chloroprocaine as amide, when it is of course an ester, distinguishing itself from the more common amides--lidocaine, bupivacaine etc...
A portion of training video includes a video produced by Dr. Vlad Frenk at the Stanford school of regional anesthesia "A Ultrasound Guided Fascia Illiaca - http://www.SsraOnlineCme.com" The direct Youtube link is HERE
See below for an example of a drop-down template for ultrasound-guided emergency nerve block. This is what we now use at Highland. Further down there is a generic checklist; it basically covers the basics of a safe ED block. The documentation sheet relates more toward the technical details of a safe block.
Peripheral Nerve Block Procedure Template
Pre-procedure neurological exam findings:
A neurologic exam was conducted including motor and sensory testing of the [free text] nerve. There were no deficits. [The following deficits were found: [free text]]. Extremity compartments were [soft, tense, not assessed].
Procedure:
A right [left][superficial cervical plexus, brachial plexus-interscalene, brachial plexus-supraclavicular, brachial plexus-axillary, radial, median, ulnar, femoral, saphenous, popliteal sciatic, posterior tibial, intercostal, greater auricular, [free text]] nerve block was performed. The patient was [was not] maintained on continuous cardiac and pulmonary monitoring throughout the procedure.
The area of injection was prepped with chlorhexidine [betadine]. Sterile technique was observed using: [+] sterile gloves, [+] sterile ultrasound probe cover, [+] sterile drape, [+] cap, [+] face mask.
A [25, 22, 20, 18 [free text]] gauge [hypodermic, quincke tip, blunt tipped block, Touhy [free text]] needle, [free text] mm in length, was used. Ultrasound guidance with real-time visualization of the needle tip was [was not] utilized throughout the procedure using an in-plane [out-of-plane] approach.
Approximately 5 [1, 2, 3, 4, 6, 7, 8, 9, 10, 15, 20, 25, 30] mL of 1 [0.5, 2, 3] % lidocaine without epinephrine [lidocaine with epi, bupivacaine, chloroprocaine] was injected near the nerve structure. Local anesthetic was [was not] gradually injected in small aliquots of 3-5 mL following negative aspiration. Low-pressure injection was confirmed using [manometer, compressed air technique]. A peripheral nerve catheter was [was not] left in place and dressed.
There was no [was] significant pain or paresthesias during the procedure. There were no [were] signs of local anesthetic toxicity. There were no [were] other complications. [free text]
Following the procedure, the blocked extremity was [was not] protected [positioned] to prevent injury and was marked with provider initials and time of the block.
Regional Block Procedural Checklist
1) Patient is identified, 2 criteria. Appropriate identifying data entered in ultrasound machine.
2) Allergies and anticoagulation status are reviewed.
3) Consent for block and any associated procedure is confirmed.
4) Appropriate neurologic and vascular exam completed and documented.
5) Block plan is confirmed*, site is marked.
6) Necessary equipment is present, drugs are labeled.
7) Resuscitation equipment is immediately available: airway devices, suction, vasoactive drugs, lipid emulsion.**
8) Appropriate monitors are applied; intravenous access, sedation, and supplemental oxygen are provided, if indicated.
9) Aseptic technique is used: hand cleansing is performed, and sterile gloves are used.
10) “Time out” is performed before needle insertion.
*Block plan should include complementary balanced analgesia and anxiolysis, appropriate matching of block to procedure/injury, appropriate timing of the block placement for optimal benefit, acquisition of block ultrasound image, post-block monitoring and care, and consultation with collaborating services involved with patient care.
**Intralipid 20% is stocked in ED room 8 Pyxiss
We know regional anesthesia works. More than that it is the perfect fit for the acute injuries and procedures we see in the ED. The technical challenges are substantial but mastered with practice and study. The big challenge ahead is developing systems that can deliver timely comprehensive acute pain management to ED patients that utilizes regional anesthesia to its fullest potential.
Our group just collaborated with the chief of our department of orthopedics to publish a description of our system at Highland. HERE

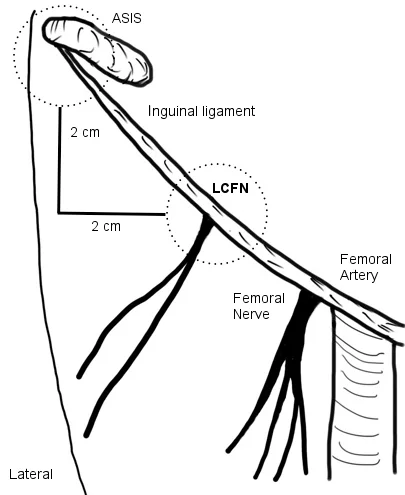
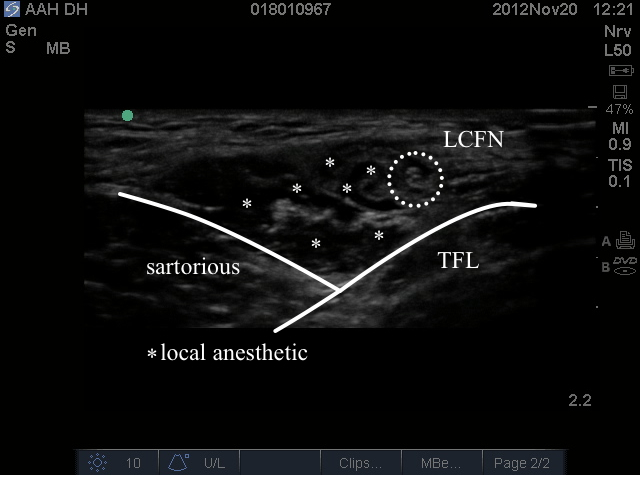
This is a very superficial block that provides sensory anesthesia and analgesia to the lateral thigh. The lateral femoral cutaneous nerve (LCFN) is a terminal branch of the lumbar plexus and enters the leg overlying the sartorious muscle. It is most often found approximately 1-2cm medial and 1-2cm inferior to the ASIS. We have have several recent cases of patients with large abscesses of the thigh where they skin pop heroin that have been successfully drained with this block.



The set up

The anatomy


High pressure ( resistance to injection ) can be the only indicator of an intramural injection. Ban Tsui has developed and validated a simple method of pressure monitoring.
1 - draw up an extra column of air in the local anesthetic syringe
2- hold the syringe vertically so that the local is dependent and the column of air is siting on top between the local anesthetic and the syringe plunger
3- The column of trapped air acts like a cushion. If you have to push with force and the air is compressed by 50% or more, stop injecting because that pressure ( about 1 atm) is way too high and associated with injurious intramural injection.
